Dental implants, whether endosteal, subperiosteal, or mini, provide stability and an aesthetically pleasing result. Following thorough treatment planning and possible preparatory steps, surgeons will use a surgical guide for precise implant placement directly into your jawbone. It's critical to nurture the health of your gums and jawbone during the subsequent osseointegration period lasting 2-4 months, where the implant bonds with your jawbone. You'll then receive an abutment and crown. To guarantee a smooth recovery, maintain good oral hygiene, stick to a nutrient-rich soft diet, and attend regular check-ups for monitoring. Initiating this path, further wisdom awaits on dental implants.
Key Takeaways
Dental implants types include subperiosteal, mini, endosteal, individual, and full-mouth, each with unique characteristics and suitability factors.
The implant procedure involves preparatory steps, precise drilling, implant placement, and fitting of an abutment and crown, using specialized equipment.
Osseointegration, the bonding of the implant to the jawbone, is crucial for implant stability and success, typically occurring over 2-4 months.
Post-procedure care includes immediate post-surgery measures, bone healing monitoring, regular dental hygiene, dietary considerations, and regular check-ups.
Factors influencing implant success include patient's age, overall health, oral hygiene, surgical procedure type, and adherence to post-procedure care guidance.
Understanding Dental Implants Types
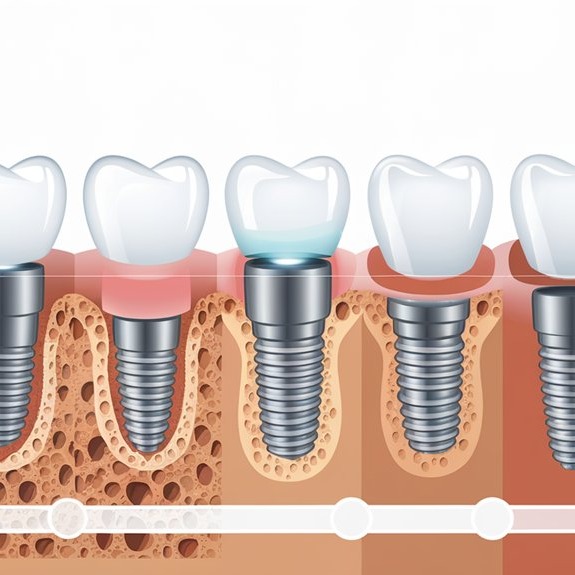
When considering dental implants, understanding the different types is essential to making an informed decision. Subperiosteal implants, for instance, offer unique advantages. These are custom-fit metal frames placed under the gums but on top of the jawbone, suitable for patients with insufficient jawbone density. The subperiosteal benefits include enhanced stability, longevity, natural fit, and the elimination of the need for bone grafting.
On the other hand, you have mini implants, which are smaller and narrower compared to standard implants. Used primarily to stabilize lower dentures, they are an ideal choice for individuals with insufficient space between tooth roots or insufficient bone density. They're less invasive and allow for quicker recovery.
Implant arrangements can be tailored to individual needs, from individual tooth implants to full-mouth dental implants. The size and location of the implants will depend on your oral health history and healthy bone availability.
When it comes to implant placement procedures, there are two main types: two-stage and single-stage implants. The former involves two separate surgeries with a healing period in between, while the latter is a one-step procedure. Both require careful post-procedure care for successful results.
Exploring Endosteal Implants

Explore the world of endosteal implants, a predominant choice in the domain of dental implantology. These implants are artificial teeth, typically made of titanium or ceramic, and placed directly into your jawbone. They're designed to replace missing teeth, providing a stable base for dental prostheses like crowns, bridges, or dentures.
The endosteal implant benefits are numerous. They can last a lifetime with proper care, offer a natural look and function, and boast a high success rate of approximately 95%. Additionally, they help preserve the integrity of your jawbone and prevent surrounding teeth from shifting.
However, understanding endosteal implant risks is equally important. The procedure can be invasive, and it requires sufficient jawbone density, which might not be present in all patients. Allergic reactions, particularly to titanium, are another concern. Smokers, too, face higher failure rates due to compromised oral health.
To qualify for this procedure, you should have excellent oral and general health, healthy gum tissue, and enough jawbone density. The recovery period typically spans several months but is usually managed with minimal pain. Regular check-ups and good oral hygiene practices are key to maintaining your endosteal implants in the long run.
Studying Subperiosteal Implants

Delving into the domain of subperiosteal dental implants, you'll find this option proves beneficial, particularly for those lacking sufficient jawbone density. Used to support artificial teeth, these implants are placed above the jawbone, beneath the gum tissue, and consist of a metal framework custom-fitted to your jaw.
The Subperiosteal Benefits are numerous. To begin with, they eliminate the need for bone grafting, making the process quicker and less invasive. They're ideal if you have insufficient jawbone density, and aren't a candidate for traditional implants. Additionally, the metal frame is custom-made to fit your jaw, ensuring a stable and natural-looking result. They replace one or multiple missing teeth and are easy to maintain, just like natural teeth.
However, Subperiosteal Risks should also be considered. The procedure is more invasive, causing more pain and a longer recovery time. There's a higher risk of infection, and they're suitable only for patients with insufficient bone density. The implants can also be more expensive due to the complexity of the surgical procedure and custom fabrication, and there's limited long-term data on their effectiveness and longevity.
The Dental Implant Procedure

Now, let's move on to the actual dental implant procedure. You'll learn about the steps involved in placing the implant, the importance of a process called osseointegration, and how the abutment and crown are attached. Understanding these key components will give you a clearer picture of what to expect during this transformative procedure.
Implant Placement Steps
Before diving into the procedure of dental implant placement, it's vital to understand the preparatory steps involved. These steps are essential to guaranteeing a successful implantation, and they involve a series of implant preparation techniques.
Diagnostic Tests: These tests assess your oral health to verify you're a suitable candidate for implants.
Treatment Planning: This is an all-encompassing session where your dental professional determines the best course of action for your unique case.
Extractions and Bone Grafts: If necessary, prerequisite procedures like extractions and bone grafts are carried out.
Particularly significant is the creation of a surgical guide, showcasing the surgical guide's importance in directing the surgeon for precise drilling of your jawbone.
Only after these steps are completed can the actual implant placement surgery commence. It involves making an incision in your gum, drilling a hole in your jawbone, and placing the titanium implant. Your gum is then stitched back together, and a healing period commences.
Abutment and Crown Attachment
Once your jawbone has fully integrated with the implant, the next phase of your dental implant procedure commences: the attachment of the abutment and crown. The abutment, a connector piece attached to the implant screw, provides a stable foundation for the artificial tooth and connects the implant to the crown. The type of abutment used depends on your specific needs and dental situation. After abutment placement, you'll require an additional healing period, typically around two weeks.
Next, a temporary crown is placed on the abutment to maintain aesthetics and functionality, while your permanent crown is being fabricated. This custom-fit temporary solution is worn for approximately six weeks.
Once ready, your permanent crown, crafted using impressions of your teeth and mouth, is attached to the abutment. Two main attachment methods exist: screw-retained and cemented crowns. The crown's material and attachment method, whether screw-retained for easy adjustability or cemented for a more permanent solution, will depend on various factors including aesthetics, durability, removability, and longevity. Ultimately, the decision is tailored to your individual situation and preferences.
Importance of Osseointegration
You might be wondering why osseointegration is such a pivotal stage of the dental implant procedure. Osseointegration significance lies in its role as the bedrock for implant healing and success. This process involves the fusion of the dental implant with your jawbone, leading to a stable foundation for your new tooth.
Hemostasis: This is the initial stage where a blood clot forms around the implant, laying the foundation for healing.
Inflammation: Next, your body's natural response to injury kicks in, preparing the site for new bone growth.
Proliferation and Remodeling: These final stages see new bone formation between the threads of the implant and the integration of the implant with surrounding tissues.
Not unlike the fusion of sounds in a genre blending music piece, each stage of osseointegration plays a critical role in ensuring the implant's long-term stability. Any disruption to the process could compromise the success of the implant. Hence, it is crucial to follow all aftercare instructions from your dentist during the healing period. Understanding the importance of osseointegration will help you appreciate the intricacies involved in achieving a successful dental implant.
Essential Dental Implant Equipment

Understanding the right equipment is essential when it comes to dental implants. As a patient, you may not need to know every detail, but a basic understanding can help you feel more at ease. The process involves various surgical instrument types and implant placement tools.
Let's start with the surgical instruments. Anesthetic syringes, surgical blade holders, periosteal elevators, tissue forceps, and needle holders are all vital for a successful procedure. These tools help in making precise incisions, handling soft tissues, and administering local anesthetics.
The next set of tools are directly involved in implant placement. Drill kits, implant drivers, healing abutments, bone mills, and retractors are all part of the toolbox. They're used for tasks like preparing the bone site, placing and securing the implants, and exposing the surgical site.
Lastly, there are diagnostic and planning tools. These include digital implant planning software, surgical loupes and microscopes, implant stability measurement devices, digital shade matching devices, and dental lasers. Each of these tools plays a specific role in ensuring the success of your implant procedure.
Equipment Type |
Example |
Role |
|---|---|---|
Surgical Instruments |
Anesthetic Syringes |
Administer local anesthetics |
Implant Placement Tools |
Drill Kits |
Prepare the bone site |
Diagnostic Tools |
Digital Implant Planning Software |
Plan and simulate the implant process |
Surgical Instruments |
Tissue Forceps |
Handle soft tissues |
Implant Placement Tools |
Retractors |
Expose the surgical site |
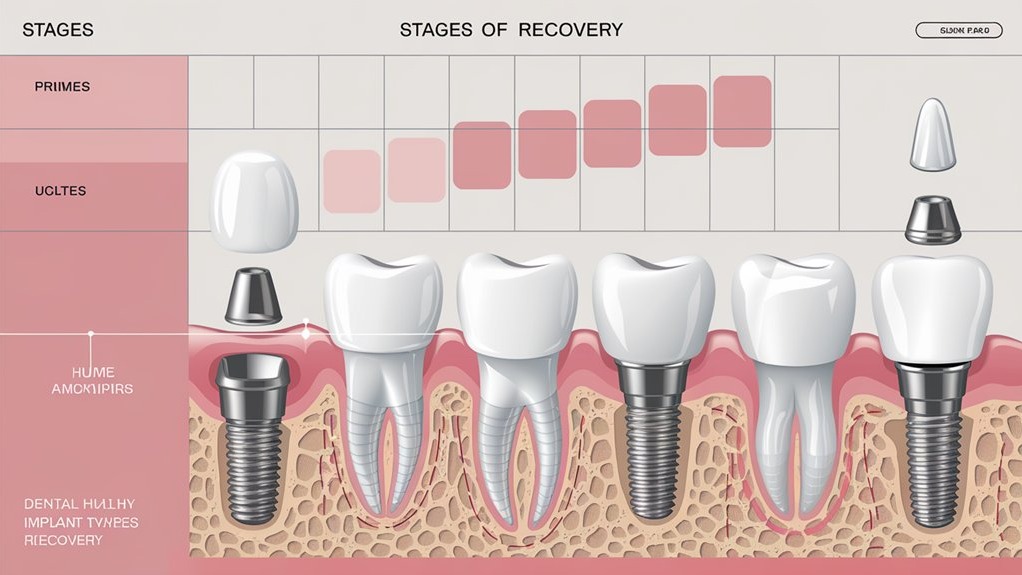
Recovery Stages From Implants
Let's now shift to the recovery stages from dental implants. From immediate post-surgery care, through the essential process of bone healing and integration, to maintaining good hygiene post-procedure, each stage plays an important role in the success of your implants. It's imperative to understand what to expect and how to aid your recovery at each juncture.
Immediate Post-Surgery Care
Post-surgery care, the cornerstone of a successful dental implant, begins immediately after the procedure. Your dentist will provide detailed post-operative instructions, which are important to follow for ideal healing and implant success.
In the initial 24 hours:
Avoid rinsing or spitting to prevent disturbing the surgical area.
Keep fingers and tongue away from the socket or surgical area to avoid infection.
Apply ice packs to the surgical area for the first 48 hours, using a 20-minutes on, 10-minutes off approach for effective swelling control.
Pain management techniques are necessary during this period. Over-the-counter medications like Tylenol or ibuprofen can manage mild discomfort, while severe pain may require prescribed medication.
Proper hydration is essential, so make sure to drink plenty of fluids. However, avoid using straws as they can create suction in the mouth, potentially disrupting the healing process.
Bone Healing and Integration
Following the immediate post-surgery care period, you'll enter the key stages of bone healing and integration, vital for the long-term success of your dental implant. This phase, also known as osseointegration, usually spans 2-4 months. During this time, the implant fuses with the jawbone, enhancing its strength and stability.
Symptoms you might experience include mild tenderness around the implant site. However, should you notice significant pain or a fever, contact your dentist immediately as these could signal complications.
Let's break down the process:
Phase |
Key Aspects |
|---|---|
Osseointegration |
Avoid hard foods, reintroduce gentle brushing and flossing, attend follow-ups |
Bone Healing |
Factors like the number of teeth replaced, age, and overall health affect healing |
Single Tooth Implant |
Healing takes 6-12 weeks, soft foods are recommended, regular check-ups are vital |
Dietary considerations and maintaining good oral hygiene are paramount during this period. The healing timeline can vary based on several factors, and it's important to be aware of the recovery challenges you might face. The patient experiences during this phase are mostly mild. Remember, proper healing and implant stability are the ultimate goals.
Post-Procedure Dental Hygiene
After undergoing dental implant surgery, your prioritized focus should be on maintaining a stringent post-procedure dental hygiene routine. It's vital to follow a few essential dental hygiene techniques to guarantee a smooth recovery and the longevity of your implants.
Regular Brushing and Flossing: It's important to brush and floss regularly, even after surgery. However, you must be gentle around the implant site to prevent any irritation.
Use of Antimicrobial Mouthwash: An antimicrobial mouthwash can help keep the implant site clean and free from infection. Make sure to follow the dentist's instructions on how and when to use it.
Professional Cleaning: Schedule regular professional cleanings with your dentist. This allows them to monitor the implant and address any issues promptly.
Incorporating these implant care tips into your routine can greatly help in the healing process. Remember, adhering to a nutrient-rich soft diet and drinking plenty of fluids is also essential for healing. Avoid hard, hot, chewy, or sticky foods, and, most importantly, smoking. Proper post-procedure dental hygiene, along with regular check-ups, guarantees the success and durability of your dental implants.
Factors Impacting Implant Recovery

The journey towards a successful dental implant involves a myriad of factors that play a vital role in your recovery. One key factor is osseointegration, the bonding of your bone with the artificial implant. This process typically takes four to six months, and in certain cases, may require bone grafts.
The surgical procedure you undergo also impacts your recovery. For instance, a two-stage implant procedure, where the implant is placed first and the abutment and temporary restoration are attached later, can extend your recovery time. The number of implants, presence of incisions, and the need for bone or soft tissue grafts can add to your recovery challenges.
Your age, overall health, and oral hygiene greatly affect your implant healing time. In special circumstances, immediate implants or single-stage procedures may reduce your recovery time, provided you are a suitable candidate.
Post-implant, your initial healing can take two weeks, with full recovery ranging from three to six months, depending on your specific case. During this period, regular follow-ups with your dentist are essential to guarantee proper healing. Remember, each patient's recovery journey is unique, so patience and diligence are key.
Post-Procedure Care Guidance

Steering through the healing process of a dental implant might seem intimidating, but with the right post-procedure care, you're already halfway there. It's vital to take specific post-surgery precautions to guarantee a smooth recovery and minimize complications.
Pain Management: Following the surgery, mild discomfort is expected. Using over-the-counter pain relievers or prescribed medications can help manage this. Remember, proper pain management strategies are an important part of the healing process.
Dietary Restrictions: Stick to soft, easily swallowed foods and cool drinks for the first few days. This precaution protects the surgical area from unnecessary stress and promotes healing.
Oral Hygiene: While spitting or rinsing should be avoided for 24 hours post-surgery, a warm saltwater rinse can be used from the second day onwards. Gentle cleaning around the implant, using a Q-tip and appropriate cleaning solution, is recommended after a few days.
Promoting Healthy Gum Recovery
As you navigate the weeks following your dental implant surgery, your focus should shift towards promoting healthy gum recovery. Your gums heal around the implant site with new tissue growth and blood clots forming. This process, known as osseointegration, continues over several months.
Your gum health is vital to successful osseointegration and long-term implant stability. It prevents bacteria from entering the implant site, thereby avoiding infection. Maintaining healthy gums is hence essential for ensuring the success of dental implants.
To support this healing process, your diet plays a significant role. Healing nutrition, rich in vitamins and minerals, particularly Vitamin C and calcium, goes a long way in supporting your gum health. Stay hydrated and avoid tobacco products to further boost recovery. Consuming foods high in antioxidants and omega-3 fatty acids can reduce inflammation and promote healing. Conversely, try to limit sugary foods that can increase bacterial growth.
Regular dental visits are necessary to monitor your recovery. Signs of healthy gum recovery include pink, firm gums, no unusual discharge or persistent discomfort, and a tight seal around the implant. Your dental professional will guide you throughout this process, ensuring that your dental implants are a success.
Frequently Asked Questions
What Is the Cost Range of Different Types of Dental Implants?
You'll find dental implants ranging from $1,000 to over $50,000, depending on materials and location. It's essential to explore implant financing options due to these costs. Each implant type uses different, often pricey, dental implant materials.
Can Dental Implants Cause Complications or Side Effects?
Yes, dental implants can lead to complications. Like traversing a rough sea, you may encounter infection risks and even implant failure. But proper care and the right dentist can steer you towards a safe shore.
How Does Smoking or Tobacco Use Affect Dental Implant Recovery?
Smoking severely impacts your dental implant recovery. It slows healing, impairs implant integration, and increases infection risk. Tobacco's influence also compromises bone health, potentially leading to future complications and reduced implant longevity. It's best to quit beforehand.
What Alternatives Are Available if Im Not a Candidate for Dental Implants?
If dental implants aren't an option for you, consider alternatives like partial dentures or dental bridges. Both offer natural-looking solutions to replace missing teeth, while being less invasive and easily maintained. Consult your dentist for personalized advice.
Does Medical Insurance Typically Cover the Cost of Dental Implants?
Typically, your medical insurance won't cover dental implants, as they're often viewed as elective or cosmetic. However, coverage can vary, so it's important to check your policy details or consult with your provider.
Conclusion
Like icing on a cake, dental implants can complete your smile beautifully. You've now explored the types - endosteal and subperiosteal, understood the procedure, recovery stages, and the factors influencing recovery. Implants require careful post-procedure care and a focus on healthy gum recovery. Remember, your dental health is a journey. With the right knowledge and care, you're well on your way to a brighter, healthier smile.
 Add Row
Add Row  Add
Add 




Write A Comment